CARCINOMA OF LARYNX
Definition: Carcinoma of the larynx is one of the most important and common malignancy of head and neck.
Aetiology:
- Age: Usually Occurs 40 to 70 years of age.
- Sex: More common in males due to smoking and tobacco habits. Laryngeal cancer is the eleventh most common cancer in men worldwide.
- Incidence: High in India, Hongkong, Europe, low in Japan, Norway, Sweden.
Predisposing factors:
- Smoking- commonest cause.
- Tobacco chewing.
- Alcohol.
- Radiation.
- Occupational like asbestos exposure.
- Genetic susceptibility.
- Laryngeal papillomas.
- Leucoplakia.
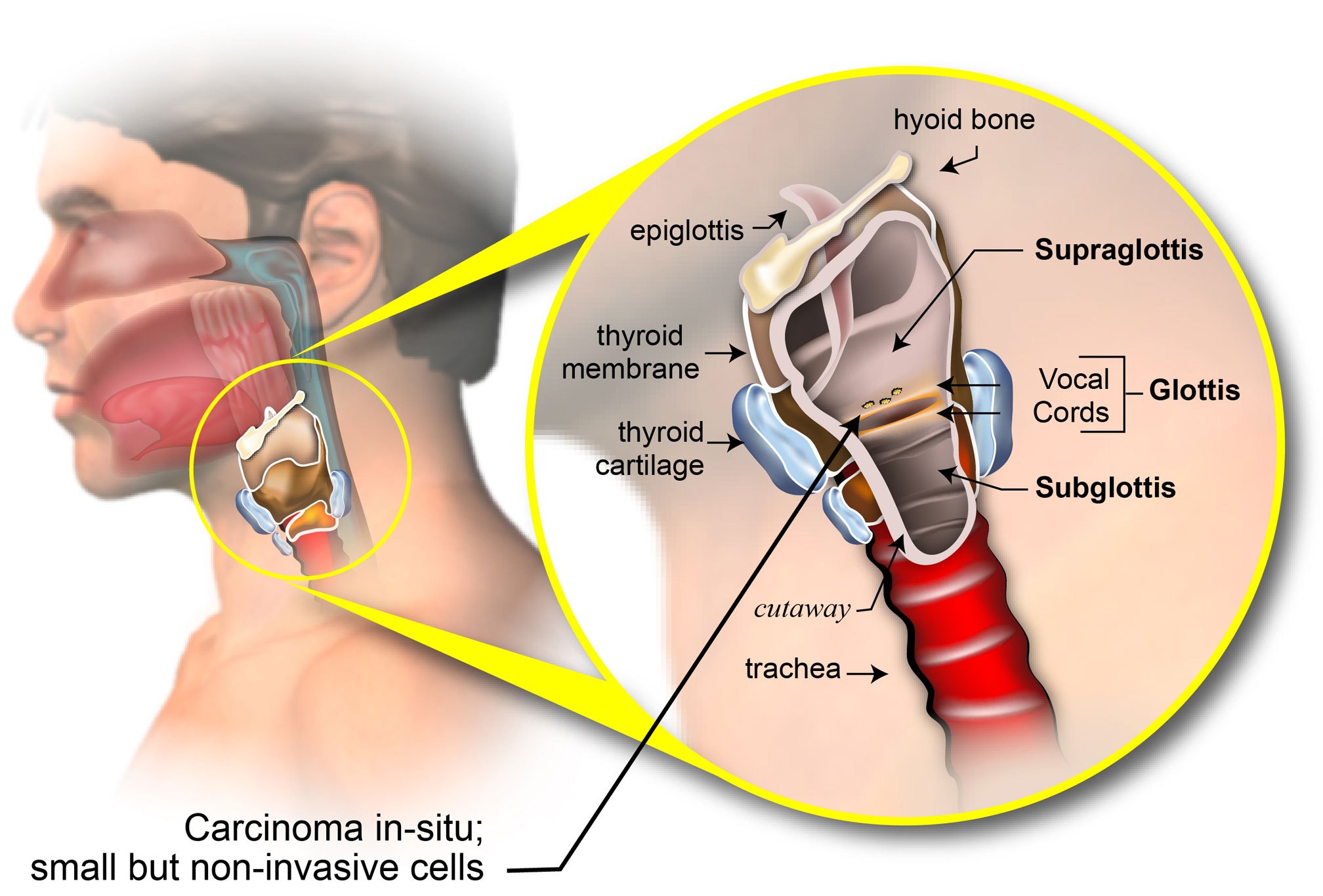
Classification:
I. According to Site:
a) Supraglottis:
- Suprahyoid epiglottis (both lingual and laryngeal surfaces).
- Infrahyoid epiglottis.
- Aryepiglottic folds (laryngeal aspect only).
- Arytenoids.
- Ventricular bands (or false cords).
b) Glottis:
- True vocal cords including 10mm below the vocal cord.
- Anterior commissure.
- Posterior commissure.
c) Subglottis:
10 mm below the free margin of vocal folds to the inferior edge of the cricoid cartilage.
d) Transglottic:
Tumours crossing or involving ventricle.
II. TNM classification:
Staging of the tumour is done or depending on the extent of the primary tumour (T), regional lymphatic involvement (N) and distant metastasis (M).
Staging:
TIS: Carcinoma in situ.
Supraglottis:
T1 Tumour limited to one subsite of supraglottis with normal vocal cord mobility.
T2 Tumour invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g., mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx.
T3 Tumour limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, pre-epiglottic tissues, paraglottic space and/or minor thyroid cartilage invasion.
T4a Tumour invades through the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of tongue, strap muscles, thyroid or oesophagus).
T4b Tumour invades prevertebral space, encases carotid artery or invades mediastinal structures.
Glottis:
T1 Tumour limited to vocal cord(s) (may involve anterior or posterior commissures) with normal mobility.
T1a Tumour limited to one vocal cord.
T1b Tumour involves both vocal cords.
T2 Tumour extends to supraglottis and/or subglottis, and/or with impaired vocal cord mobility.
T3 Tumour limited to the larynx with vocal cord fixation and/or invades paraglottic space and/or minor thyroid cartilage erosion.
T4a Tumour invades through thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid, or oesophagus).
T4b Tumour invades prevertebral space, encases carotid artery or invades mediastinal structures.
Subglottis:
T1 Tumour limited to the subglottis.
T2 Tumour extends to vocal cord(s) with normal or impaired mobility.
T3 Tumour limited to larynx with vocal cord fixation.
T4a Tumour invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of tongue, strap muscles, thyroid or oesophagus).
T4b Tumour invades prevertebral space, encases carotid artery or invades mediastinal structures.
Nodes:
Nx: Regional lymph nodes cannot be assessed.
N0: No regional lymph node metastasis.
N1: Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension. Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension, or multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension, or bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension.
N1a: Metastasis in a single ipsilateral lymph node more than 3 cm but not more than 6 cm in greatest dimension.
N1b: Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension.
N1c: Metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension.
N2: Metastasis in a lymph node more than 6 cm in greatest dimension.
Metastasis:
Mx Distant metastasis cannot be assessed.
M0 No distant metastasis.
M1 Distant metastasis.
Histopathologic grading (G):
Grade 1: Well-differentiated.
Grade 2: Moderately differentiated.
Grade 3: Poorly differentiated.
Symptoms:
- Hoarseness of voice is the commonest symptom.
- Stridor, cough, haemoptysis.
- Neck swelling.
- Dysphagia (Pyriform fossa and post cricoid involvement).
Investigations:
- Indirect laryngoscopy.
- Direct laryngoscopy this can be done along with a biopsy of the tumour mass and visualisation of the extent.
- Fibre-optic laryngoscopy.
4. Stroboscopy- Stroboscopy is a special method of examination of the vibrations of vocal folds. A bright flashing light lasting a fraction of a second (10µs) is used to illuminate the vocal folds. This flash ‘freezes’ the movement of the vibrating vocal folds. By taking multiple snapshots at different phases of the vibratory cycle it is possible to see details of the change in shape of pliable surface of the vocal folds (i.e. the mucosa) with time.
5. CT scan- Evaluation of laryngeal squamous cell carcinoma requires a contrast CT study of the neck. Excellent images of the neck are obtained using a multidectector CT (MDCT) following the injection of an iodinated contrast agent (total dose 35-40 g). Axial scanning is performed from the skull base to the aortic arch with the acquisition plane parallel to the plane of hyoid bone, to obtain scans parallel to the true vocal cords. An additional examination for better assessment of the tumor in laryngeal ventricle, anterior commisure and aryepiglottic folds may be done with e-phonation.
6. MRI scan- A high field MRI scanner using a dedicated neck coil is preferred. A combination of multiplanar non-contrast T1-weighted, T2-weighted and T2-weighted fat saturation images with postcontrast T1 fat-suppressed images are routinely used. It is important to take the T1 and T2 sections at the same levels. A section thickness of 4 mm is preferred with an interslice gap of 0-1 mm.
CT and MRI play a significant complimentary role to clinical endoscopy in staging of laryngeal SCC. Determination of the precise extent of cancer spread within the larynx (T staging) is the single most critical factor guiding treatment decisions in patients with localized laryngeal cancer. Additionally, imaging studies are routinely used to assess associated nodal disease (N staging) and systemic metastases (M staging), presence of synchronous cancers and also post-therapeutic tumor recurrence in these patients.
7. PET/CT imaging- It is useful in laryngeal tumors in cases of suspected locoregional recurrence where conventional imaging (CT and MRI) is unable to resolve the diagnostic doubt.
Treatment:
The treatment for laryngeal cancer largely depends on the stage of the cancer. The main treatments are radiotherapy, surgery and chemotherapy.
1.Stage 0
- These cancers are almost always glottic (vocal cord) cancers and are detected early due to change of voice. They are nearly always curable with either endoscopic surgery (Laser Cordectomy) or radiation therapy (5000-8000 rads are divided over a period of 6-8 weeks). A regular follow up is required to detect any recurrence. In cases of recurrence radiation is preferred.
- Almost all people at this stage can be cured without major surgery. Risk factors like smoking increase the recurrence rate.
2. Stage I and II laryngeal cancers
- Most people with stage I and II laryngeal cancers can be treated successfully without totally removing their larynx.
- Either radiation alone (without surgery) or partial laryngectomy can be used in most people. Radiation therapy is used for smaller cancers. Voice quality is better after radiation therapy than with partial laryngectomy.
- The treatment for glottic (vocal cord) cancers and supraglottic cancers (those starting above the vocal cords) is slightly different. Some early glottic cancers may be treated by removing the affected vocal cord with (cordectomy)
- Radiation or surgery is usually enough to treat most glottic cancers. Chemoradiation, or surgery may be used to residual or recurrent disease.
- Supraglottic cancers are more likely to spread to the neck lymph nodes. Surgical removal of tumour is done by supraglottic laryngectomy and a simultaneous neck lymph node dissection done. If treatment is radiation therapy alone, then radiation to the lymph nodes in the neck is also given.
3.Stage III and IV laryngeal cancers
- The main options for initial treatment for these cancers are surgery or chemotherapy with radiation. Radiation therapy alone (or with the targeted drug cetuximab) may be an option for people who cannot tolerate surgery. Immunotherapy might be another option for some people with stage IV cancer.
- Surgery for is almost always complete removal of the larynx (total laryngectomy) but a small number of these cancers might be treated by partial laryngectomy.
- These tumours have a higher risk of lymph node metastasis in the neck. Hence these lymph nodes are cleared by radical neck dissection. Radiation therapy with chemotherapy may be needed after surgery, especially if the disease has spread to the lymph nodes.
- In cases of extra laryngeal spread to surrounding structures the only surgical treatment option is total laryngectomy along with removal of the adjacent involved tissue like thyroid gland.
- Induction chemotherapy is given sometimes to shrink the tumour. If the tumour doesn’t shrink, surgery is usually the next treatment.
- Cancers that are too big or have spread too far to be completely removed by surgery are often treated with radiation, usually combined with chemotherapy or cetuximab. Another option might be treatment with an immunotherapy drug, either alone or with chemotherapy. Sometimes, if the tumour shrinks enough, surgery of lymph nodes in the neck may be done. But for many advanced cancers, the goal of treatment is often to stop or slow the growth of the cancer for as long as possible and to help relieve some symptoms.
We Are Always Ready to Help You.
Book An Appointment

