CHRONIC MAXILLARY SINUSITIS
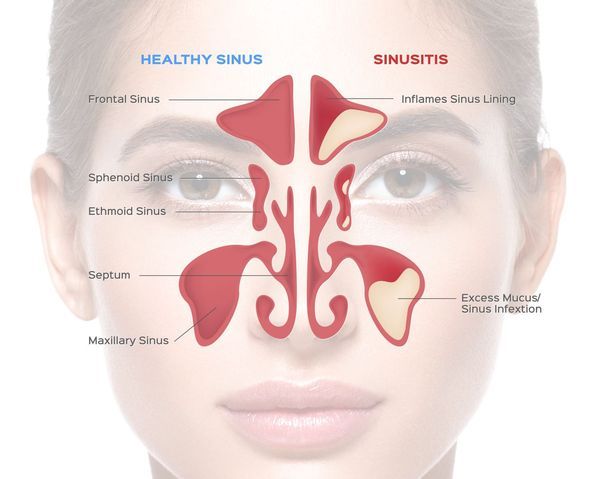
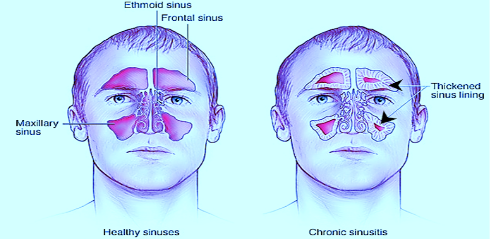
Definition- The maxillary sinuses are the most commonly affected sinuses because its ostium is at the higher level than the base of the sinus. Chronic maxillary sinusitis is usually a result of improperly treated recurrent acute sinusitis.
It is called chronic when duration of symptoms is more than 12 weeks duration and there are inflammatory changes on imaging more than 4 weeks after starting appropriate medical therapy.
Aetiology:
- Age: Usually occurs after 16 years of age.
- Sex: Both sexes are equally affected.
- Mechanical obstruction of the ostium of the Maxillary sinus results in improper drainage of the sinuses.
a) Deviated nasal septum causing blockage in the mucociliary clearance pathway of the maxillary ostium.
b) Hypertrophied turbinates.
c) Adenoid hypertrophy.
d) Tumors of nose and maxilla.
e) Foreign bodies, rhinolith. - Allergic rhinitis: The mucosa becomes oedematous and blocks the ostium.
- Mucociliary clearance abnormality of the sinuses.
- Immune deficiency.
- Chronic tonsillitis and infected upper molars and premolars.
- Hormonal imbalance.
Causative organisms:
Gram-negative organisms include:
- Moraxella catarrhalis.
- Haemophilus influenzae.
- Prevotella species.
- Enterobacter species.
- Pseudomonas species.
- Streptococci.
- Coagulase-negative staphylococci.
- Staphylococcus aureus.
It is believed that the main species involved in the exacerbation of sinusitis and nasal polyps is Staphylococcus aureus which harbours genes coding for enterotoxins.
Pathophysiology:
Chronic Maxillary Sinusitis is subcategorized into with polyps and cases without polyps.
Chronic Maxillary Sinusitis without nasal polyposis is characterized by:
- Intense oedematous stroma in the sinonasal epithelium, with albumin deposition, pseudocyst formation and subepithelial or perivascular inflammatory cell infiltration.
- It is associated with a typical T-helper 2 cell (TH2) skewed eosinophilic inflammation, with high interleukin (IL-5) and eosinophil cationic protein (ECP) concentrations in the polyps.
- Fibrosis, basement membrane thickening, goblet cell hyperplasia, subepithelial oedema, and mononuclear cell infiltration.
- It exhibits a T-helper 1 cell (TH1) milieu, with increased levels of interferon gamma (IFN-γ) in inflamed sinus mucosa and low ECP/ myeloperoxidase ratios.
Clinical features:
Symptoms
Symptoms
- Nasal discharge: Usually mucopurulent. Discharge may trickle posteriorly to the pharynx. Dry cough may be present due to post nasal discharge.
- Hyposmia may occur.
- Nasal blockage on the affected site due to oedematous nasal mucosa.
- Loss of nasal resonance.
Signs:
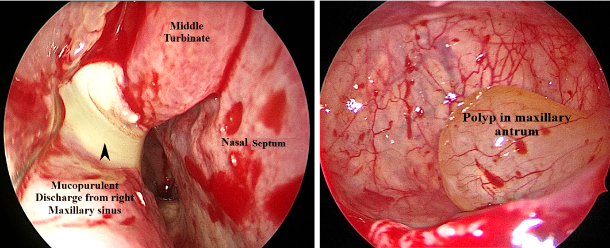
- Anterior Rhinoscopy may reveal discharge along the middle meatus area.
- Posterior Rhinoscopy reveals post nasal discharge.
- Transillumination test shows opacity in the maxillary sinus.
- Clinical Examination / anterior rhinoscopy.
- X-ray of PNS: Waters view and Caldwell’s view.
- CT Scan of paranasal sinuses - Axial, Sagittal and Coronal sections.

4. Diagnostic nasal endoscopy.
Diagnostic criteria
Diagnostic criteria
| Diagnostic criteria of Chronic Maxillary Sinusitis | Symptoms should be correlated by either endoscopic and/or radiological findings |
| Duration | >3 months |
| Primary symptoms (requires at least one to be present ) | Nasal blockage/obstruction/ congestion Nasal discharge (anterior/ posterior). |
| Additional symptoms (may also be present and at least one is needed if only one of the primary symptoms is present)- | Facial pain/pressure Olfactory dysfunction Hyposmia/anosmia |
| Endoscopic findings (any of these)- | Nasal polyps Mucopurulent discharge (middle meatus) Oedema/mucosal obstruction in middle meatus. |
| CT scan findings (as well as or instead of endoscopic findings- | Mucosal changes within the osteomeatal complex and/or sinuses. |
Treatment:
Treatment can be divided into medical and surgical and it aims to:
- Eliminate symptoms and nasal polyps.
- Re-establish nasal breathing and olfaction.
- Prevent recurrence and improve quality of life.
- Medical treatment consists mainly of topical and systemic corticosteroids.
➣ It effects eosinophil function directly by reducing both eosinophil viability and activation and indirectly by reducing the secretion of chemotactic cytokines by nasal mucosa and polyp epithelial cells.
➣ The effect of nasal spray on sense of smell is poor when compared to systemic steroids, which may be due to the sprays being unable to reach the olfactory mucosa because of oedema.
➣ Nasal drops are more effective than sprays and have a significant positive effect on sense of smell.
➣ Topical steroids may be used but not more than 2 months at one time unless under specialist supervision or for not longer than 4 months in one 12-month period, as they can be absorbed systemically.
➣ Larger polyps may require systemic corticosteroids like prednisolone 0.5 mg/kg each morning for 5–10 days. Maintenance therapy with topical corticosteroid spray is recommended as these may have lower bioavailability than drops. - Antihistamines can be given if allergy is present.
- Leukotriene inhibitors help patients with coexisting asthma and/or aspirin sensitivity.
- Antibiotics- For chronic recurrent sinusitis, a 3-month course of a macrolide antibiotic can help nasal polyps. Macrolides have been shown to increase mucociliary transport, reduce goblet cell secretion and causes reduction of chronic inflammation. However, acute cardiac toxicity is an increasingly recognized potential adverse effect.
Surgical Management
➣ Functional endoscopic sinus surgery aims to improve sinus ventilation and drainage as well as removing polyps. The extent of surgery varies with the extent of disease, the surgeon’s individual practice and available technology.
➣ Postoperatively, patients should be treated with nasal douching and intranasal or systemic corticosteroids.
➣ Postoperatively, patients should be treated with nasal douching and intranasal or systemic corticosteroids.
We Are Always Ready to Help You.
Book An Appointment

